Feed Item
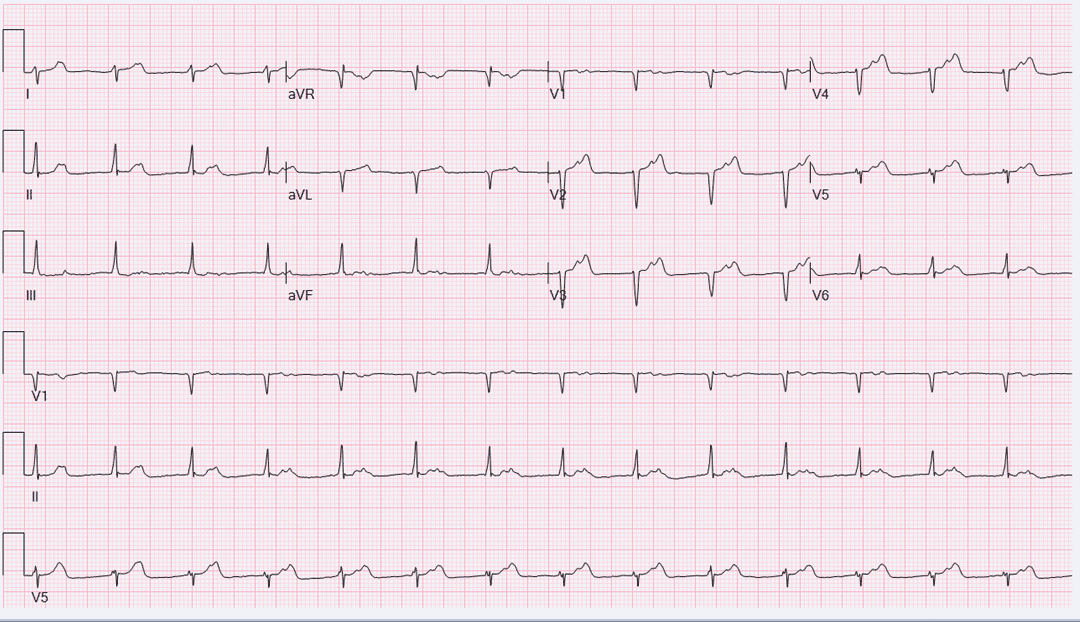
87-year-old male complains of dyspnea on exertion worsening over last 6 months, PND, orthopnea, and lower limb edema improved with diuretics. ECHO showed preserved LVEF, diastolic function not adequately assessed. ECG is shown below.
•What is the next best step?
1- Continue diuretics
2- Start ACE inhibitors
3- Implant dual chamber pacemaker
Comments


F
Rhythm is regular (relatively narrow) with rightward QRS axis around +100-110. Q waves anteriorly suggestive of possible old anteroseptal MI. It will be helpful to see an older EKG, so axis can be compared as it is uncommon to see this rightward axis at this age, and if this is significant the shift can be assumed due to left posterior fascicular block.
QRS are not preceded by immediate P waves, but there is consistent P waves seen in the ST segment of prior beats with PR interval over 500 ms. The morphology of these P waves in inferior leads are not very clear to discern if they are antegrade or retrograde, but they are likely antegrade (given their width). In which case, the rhythm is sinus with very long PR interval making atrial kick likely occurring during prior ventricular systole; hence can explain the patient's SOB (with data to support PM implantation will improve symptoms).
At the bedside, it will be interesting to see regular "Cannon" waves on JVP evaluation.
Option: 3 dual chamber pacemaker
The presence of low voltage with pseudo infarct pattern as well as heart failure with preserved EF/conduction abnormalities might be related to underlying cardiac amyloidosis. Although, I am expecting to see other supportive findings on echocardiogram Including diastolic dysfunction.
The P wave morphology appears to be positive in lead II which supports sinus origin.
if I may ask, is there a cutoff PR interval for AV conduction to occur?
The second question to Dr. Fathi Idris,
How does the width of the P wave help to decide if it is retrograde vs antegrade?
Thank you Dr. Yousef Darrat for sharing with us this case.
F
Although voltages are "lowish" in general, but not sure if they meet the criteria of "low voltage" (all limb leads <5mm and all precordial <10mm).
Agree, P wave is probably sinus (but sometime when it is on T, you need to be careful).
In general, retrograde P waves (assuming originating from a backwave below His, is usually skinny as the activation of both atria occur simultaneously starting in the septum area (in the EP lab this is easier to see). However, sinus or other atrial rhythm usually leads to a wider P waves (typically has two components) as the atria are activated sequentially.
2004 EKG is above, first degree AV block otherwise unremarkable
2018 EKG longer PR interval
Post pacemaker implant
Thanks Fathi and Mansour. Great points. Amyloidosis is a consideration and I think it is under diagnosed in daily clinical practice. MRI would be valuable here.
this patient had a pacemaker implant due to symptomatic first degree AV block. because of frequent RV pacing I decided to implant His bundle Pacemaker, patient symptoms Significantly improved after pacemaker implant I will share with you old EKGS and also EKG post ppm implant.
F
Thanks Yousef Questions/comments:
1.Although His pacing makes physiological sense, however, it is cumbersome and can be tedious. Do we have data to support superiority over RV pacing for this patient with preserved EF?
2.The pacing EKG does not look "pure" HBP. The QRS is wider than baseline EKG and there is a significant axis shirt (from right at baseline to extreme left on paced EKG), how to explain that? do you think it is capturing some other fascicular elements instead, with or without some RV? a post implant CXR will be very helpful if you have it.
3.What is HBP threshold?
Great case!