Feed Item
Would like to share this case from last week. It is an acute MI but with a couple of twists in presentation that I thought worth sharing.
A 61 year-old-male with family h/o CAD. Presented to ED with 30 min of left sided chest pain radiates to the left shoulder. EKG on arrival shown.
Initial hs-cTnT: 7 and 1-hr later was 11 (normal NTG lowered CP from 10/10 to 4/10, morphine helped as well.
Repeat hs-cTnT at 3-hr is: 41. EKG 2 hours later shown:
The patient was taken to the Cath lab and found to have a coronary lesion. Where is that lesion?
Comments

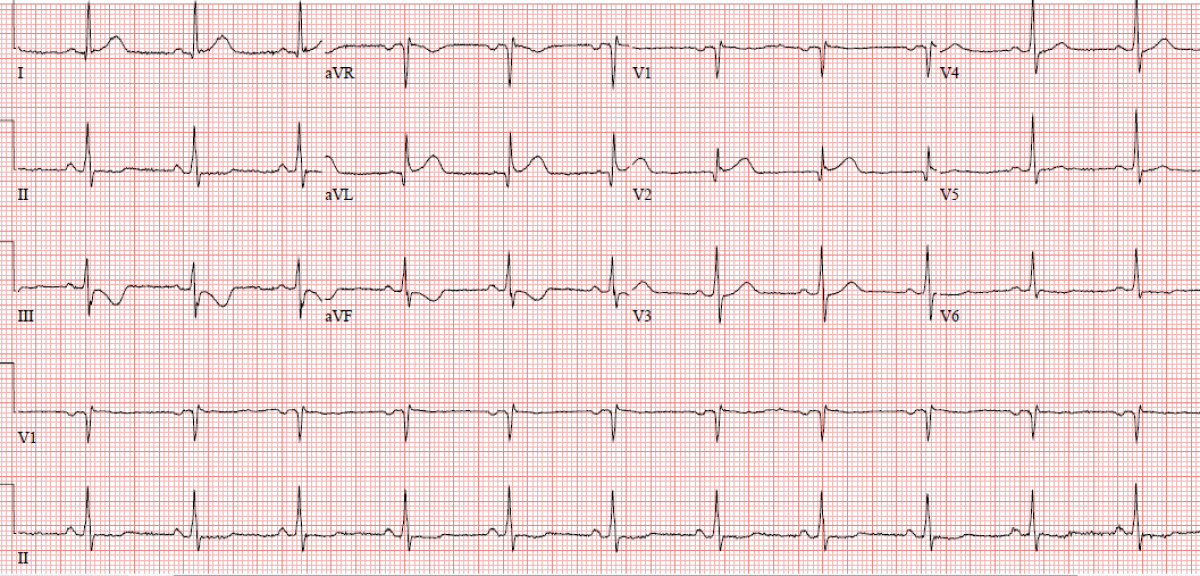
12-lead EKG showed sinus rhythm 75 bpm with ST segment elevation in the upper lateral leads (I and aVL) and V2 with reciprocal ST segment depression/T wave inversions in the inferior leads (most pronounced in lead III) consistent with diagonal/ramous intermedius branch 100% acute occlusion (South African flag sign).
I am not certain why the patient was not taken to the cath lab after the initial EKG.
Well said Mansur. Totally agreed 👌
Nice case. Findings are diagnostic for occlusion of first diagonal branch (South African Flag Sign) as Dr. Khaddr @Mansour Khaddr nicely pointed out. This is a nice article about this.
F
Perfect, you guys hit the nail on the head. Focal first diagonal occlusion. Images from before and after intervention is below. Angios films attached. The diagonal was found to have a thrombotic lesion. Post interventional flow was slightly sluggish, TIMI 2-3.
EKG post intervention below showing resolution of these changes and Q-wave progression:
Here is the next twist. 24 hr later, while he was in the hospital, he developed sudden-onset chest pain associated with diaphoresis and palpitations. He is tachycardic but BP is stable.
Repeat EKG is shown below.
12-lead EKG showed atrial fibrillation with rapid ventricular response (around 150 bpm), normal axis.
Lateral myocardial infarction, age recent (likely aneurysmal changes).
Rate control with BB and anticoagulation with heparin drip.
Chest pain will probably be better once rate controlled. If persistent chest pain after rate controlled, you might need to re-image the coronaries for stent thrombosis!! although the territory involved is infarcted and small in size.
The bite of an ant is as painful as of something .... (filling the space)!!!
Going back to her coronary angiogram: was SCAD on the differential diagnosis?
F
Thanks @Mansour Khaddr for your thorough explanation. As you indicated AF was likely the likely for his symptoms. There was some concerns about the slight ST elevation in aVL and I (not V2) to be related to stent thrombosis, and given his CP he was taken back to the cath lab and stent was patent.
In his case, the CP was pleuritic and in combination with AF it was felt this is just a post-MI pericarditis. The EKG changes were related to his recent MI, but with tachycardia the residual STE got exaggerated.
He was treated with NSAID and Colchicine and did very well.
I was surprised to see pericarditis in such a small and focal MI with very minimal elevation of troponin and early intervention.
Thank you all for your enlightening discussion.
Excellent educational case. Thank you Dr Fathi for sharing!!