An 80-year-old male presented with persistent right shoulder pain, achy in nature for the last couple of weeks. No significant improvement post local cortisone injection.
PMH: CAD s/p 4V CABG (grafts occluded except RCA graft). Coronary/graft angiogram in 5/2022 performed for similar symptoms showed RCA vein graft ostial 95% stenosis s/p PCI with resolution of his shoulder pain. Also, had balloon angioplasty only to proximal LAD in-stent restenosis as already has 2 stents at that location. He was doing well till 4-6 weeks ago when his right shoulder pain recurred. He also has CKD stage IV, PVD, carotid artery disease s/p intervention and ischemic CVA with no obvious residual weakness.
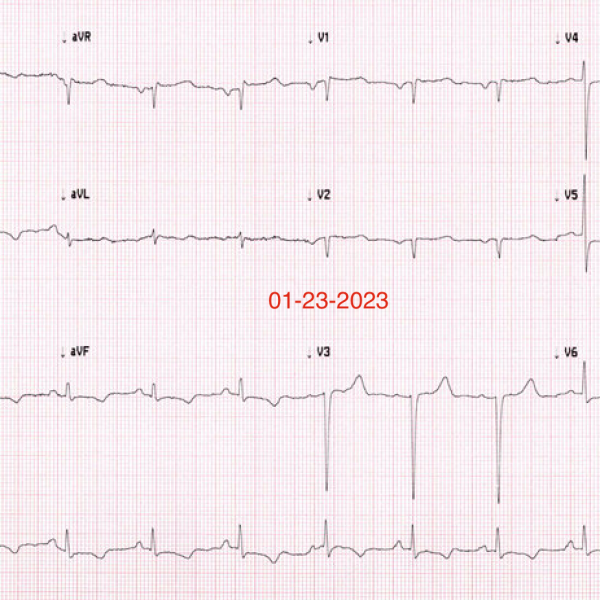
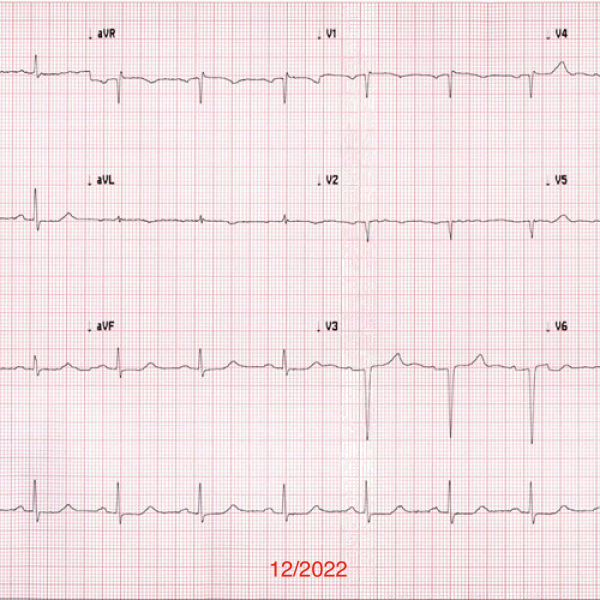
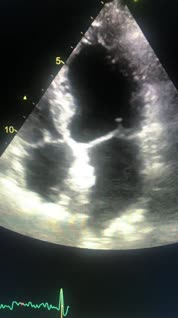
His initial EKG from 12/2022 and second EKG done this week. Also, limited echo images posted. His echo in 4/2022 showed LVEF 55% with no regional wall motion abnormality.
It is a bread and butter case. What is the echocardiogram findings?
Would like to share this case from last week. It is an acute MI but with a couple of twists in presentation that I thought worth sharing.
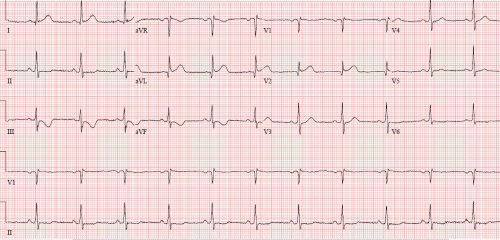
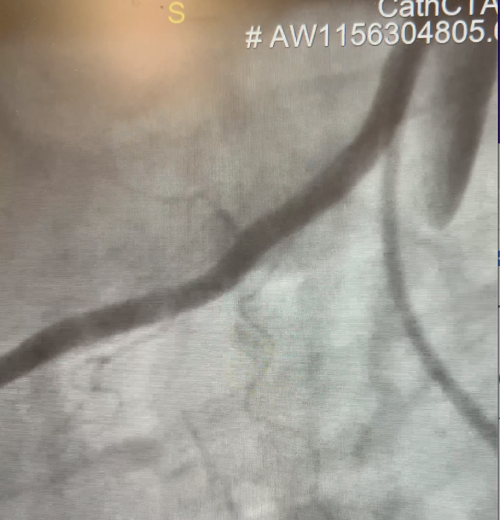
A 61 year-old-male with family h/o CAD. Presented to ED with 30 min of left sided chest pain radiates to the left shoulder. EKG on arrival shown.
Initial hs-cTnT: 7 and 1-hr later was 11 (normal NTG lowered CP from 10/10 to 4/10, morphine helped as well.
Repeat hs-cTnT at 3-hr is: 41. EKG 2 hours later shown:
The patient was taken to the Cath lab and found to have a coronary lesion. Where is that lesion?