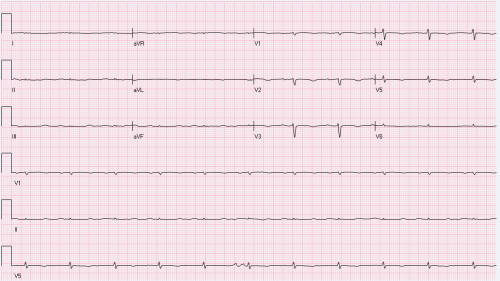
This is an EKG on 70-year-old male. He has multiple medical problems including shortness of breath, chronic kidney disease, anemia and other medical problems.
This EKG came through routine EKG reading. What 1st thing comes in mind when you see this EKG, and why?
I would like to share with you this case I saw in Nashville a couple of days ago..
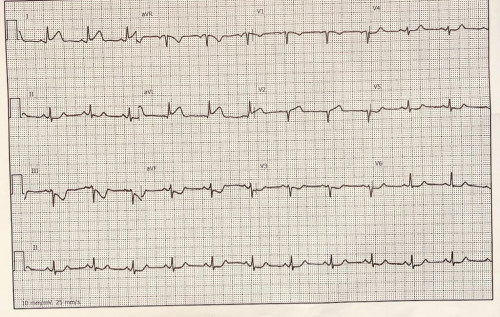
A 47-year-old Hispanic lady, presented to the Emergency department (ED) with chest pain while climbing the stairs. The pain lasted for 45 min before arrival to ED.
Her presenting EKG is shown here.
What is the interpretation of the EKG, and what we do next?
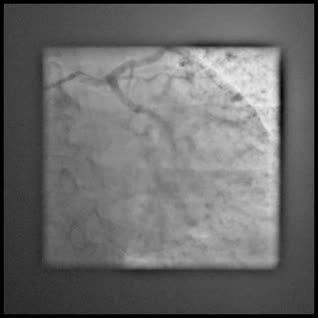
I would like to share this interesting case from couple of days ago.
A 63-year-old African American lady with acute coronary syndrome. During her catheterization, when injecting the left main coronary artery, the catheter slid and jumped into another vessel. That turned out to be the RCA originating just very close to the left main. A repeat cranial view, (angiogram 2.) Clarifies the relationship between to the separate ostia in the left coronary cusp.
CX was occluded and RCA has two proximal tandem lesions.
We elected to perform intervention on both vessels. Finding a guide catheter for the apparent RCA was a bit challenging, however we used a JR4 guide catheter but needed to engage the ostium with an interventional wire of the cusp and then advanced the JR4 guide catheter to the ostium of the aberrant RCA. The rest was straight forward.
I wonder, if we did not luckily jump in to the RCA from the left coronary cusp injection, we could have wasted long time trying to search for the RCA on the right coronary cusp. Rare anomaly, but keep it in mind!
Diagnostic Approach and Management of Hypertension - Part I (June-10-2023):
#Internal Medicine
#Preventive Cardiology
AA,
I hope you could join us this
Saturday (June 10th 2023, 7 PM Libyan time).
Title: Diagnostic Approach and Management of Hypertension.
Join Zoom Meeting
https://us02web.zoom.us/j/4029726854
Meeting ID: 402 972 6854